Herniated Disc
Herniated Disc: When Surgery Is Necessary — and When It Is Not
By Natalia Skizha
Neurosurgeon
Medical Author at Briefor Health
Herniated disc is common — surgery is not
A herniated disc is one of the most common causes of back and neck pain worldwide. For many patients, the diagnosis immediately raises fear of surgery. In reality, most disc herniations do not require surgical treatment.
Understanding when surgery is truly necessary — and when conservative management is safer and more effective — is essential for both patients and clinicians.
What is a herniated disc?
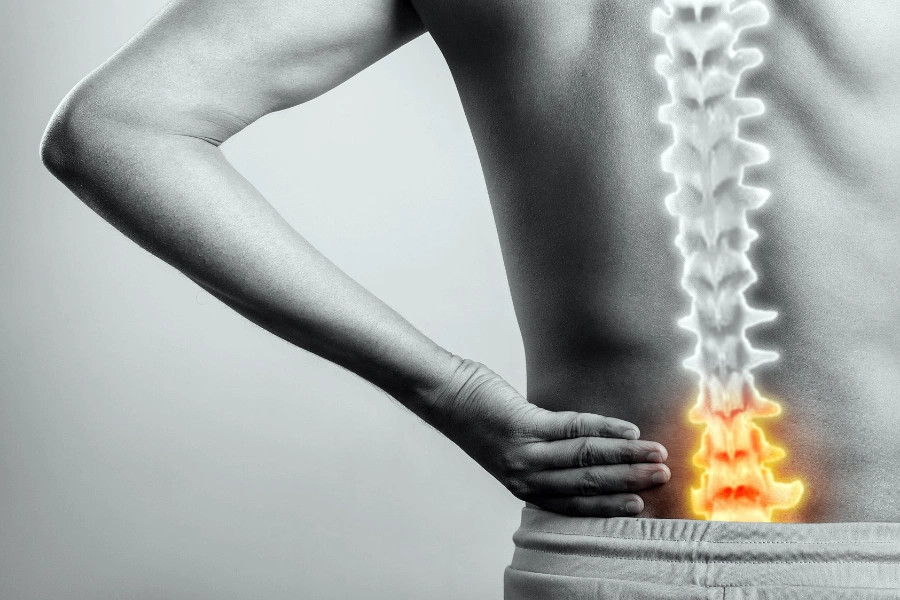
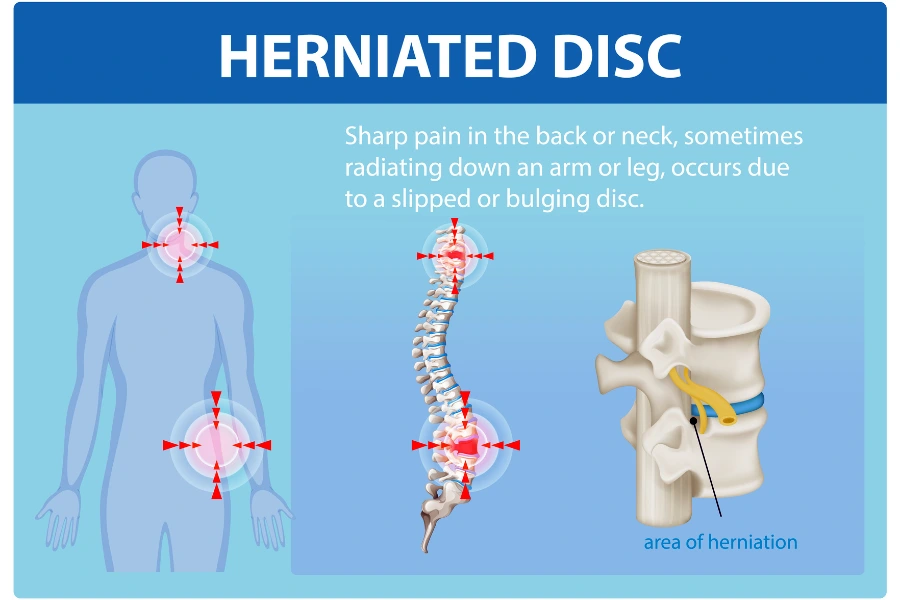
Intervertebral discs act as shock absorbers between the vertebrae. A herniation occurs when the inner gel-like nucleus protrudes through the outer fibrous ring, potentially compressing nearby nerve structures.
Depending on the location, disc herniation may affect:
- the cervical spine (neck);
- the thoracic spine (rare);
- the lumbar spine (lower back, most common).
Symptoms range from localized pain to radiating pain, numbness, weakness, or neurological deficits.
When conservative treatment is appropriate
In the majority of cases, symptoms improve without surgery.
Conservative management may include:
- activity modification;
- physical therapy;
- anti-inflammatory medications;
- targeted pain management strategies;
- image-guided injections in selected cases.
Clinical studies consistently show that up to 80–90% of patients improve within weeks to months with non-surgical treatment alone.
Time, proper diagnosis, and structured follow-up are often more important than aggressive intervention.
When surgery becomes necessary
Surgery is not decided by MRI findings alone. Clinical symptoms and neurological status are decisive.
Surgical treatment is generally indicated when one or more of the following are present:
1. Progressive neurological deficit
Worsening muscle weakness, loss of reflexes, or sensory deficits indicate ongoing nerve damage that may become irreversible.
2. Severe pain resistant to treatment
Pain that remains disabling despite adequate conservative therapy may justify surgical intervention to restore quality of life.
3. Cauda equina syndrome (emergency)
Symptoms such as bladder or bowel dysfunction, saddle anesthesia, or bilateral leg weakness require urgent surgical decompression.
4. Radiological–clinical correlation
MRI findings must clearly correspond to the patient’s symptoms. Imaging alone is never sufficient.

Why MRI must be interpreted carefully
MRI is an indispensable diagnostic tool, but it is frequently misunderstood.
Disc protrusions are often found in asymptomatic individuals, especially after the age of 40. Treating MRI images instead of patients leads to unnecessary procedures.
A neurosurgeon evaluates:
- the level and type of herniation;
- degree of neural compression;
- spinal canal dimensions;
- correlation with neurological examination.
Modern surgery is precise — but still surgery
When surgery is required, modern neurosurgical techniques aim to:
- minimize tissue disruption;
- preserve spinal stability;
- relieve neural compression efficiently.
However, surgery always carries risks and should never be the first option without clear indications.
The goal is not to “fix the MRI”, but to restore neurological function and relieve suffering.
The most common patient mistake
One of the most frequent errors is delaying professional evaluation due to fear — or, conversely, rushing into surgery after reading MRI reports without proper consultation.
Both extremes are harmful.
Correct decision-making requires:
- clinical assessment;
- imaging interpretation;
- understanding of natural disease progression;
- individualized treatment planning.
Conclusion
A herniated disc is not a surgical diagnosis by default. Most patients recover with conservative treatment, patience, and proper medical guidance.
Surgery is highly effective when truly indicated, but unnecessary surgery exposes patients to avoidable risks.
The most important step is not choosing surgery or avoiding it — but choosing the right moment and the right indication.