MRI and Back Pain
MRI and Back Pain: What Imaging Really Shows — and What It Doesn’t
By Natalia Skizha
Neurosurgeon
Medical Author at Briefor Health
MRI has changed spine diagnostics — but it has also created new misconceptions
Magnetic resonance imaging (MRI) is one of the most powerful diagnostic tools in modern medicine. In patients with back pain, it is often perceived as the definitive answer — a test that can explain every symptom and dictate the correct treatment.
In reality, MRI is a tool, not a diagnosis.
Understanding what MRI can reveal — and what it cannot — is essential for making safe and informed clinical decisions.
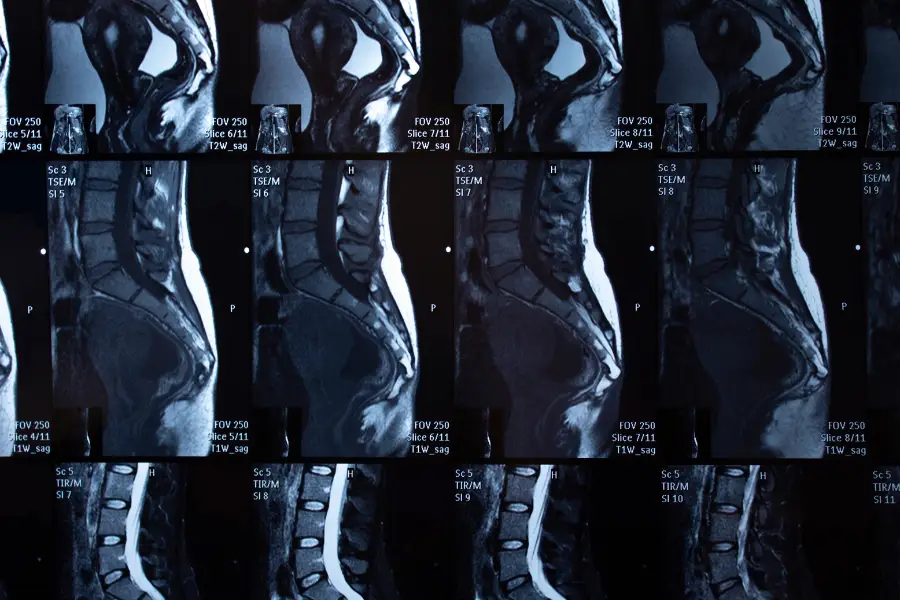
What MRI is actually designed to show
MRI provides detailed visualization of soft tissues, including:
- intervertebral discs;
- spinal cord and nerve roots;
- ligaments and facet joints;
- inflammatory or structural changes.
It is particularly valuable for identifying:
- disc herniation or extrusion;
- spinal canal stenosis;
- tumors, infections, or inflammatory processes;
- nerve compression correlating with neurological symptoms.
When interpreted correctly and in the proper clinical context, MRI is indispensable.
Why MRI findings often do not explain pain
One of the most important facts patients rarely hear is this:
Abnormal MRI findings are extremely common in people without pain.
Large population studies have shown that:
- disc bulges and protrusions are present in many asymptomatic individuals;
- degenerative changes increase with age regardless of symptoms;
- “abnormal” MRI results do not automatically indicate disease.
This means that seeing a disc protrusion on MRI does not necessarily explain back pain.

The most common MRI findings — and what they really mean
Disc bulge vs. disc herniation
A disc bulge is often a part of normal aging and does not always cause symptoms. A true herniation may or may not be clinically relevant depending on nerve involvement.
Degenerative disc disease
This term sounds alarming but usually describes age-related changes rather than a pathological condition requiring intervention.
Facet joint changes
These may contribute to pain but often coexist with other non-spinal pain generators.
Without clinical correlation, these findings are descriptive, not diagnostic.
Why “treating the MRI” is a mistake
One of the most frequent clinical errors is initiating treatment — including surgery — based solely on imaging results.
MRI does not show:
- pain intensity;
- functional impairment;
- muscle spasm;
- psychosocial contributors to pain;
- patient tolerance or adaptation.
Back pain is a multifactorial condition, and imaging captures only one part of the picture.

When MRI is truly necessary in back pain
MRI is most valuable when:
- pain persists despite adequate conservative treatment;
- neurological deficits are present or progressing;
- symptoms suggest serious pathology (infection, tumor, trauma);
- surgical or interventional treatment is being considered.
In acute, uncomplicated back pain without red flags, early MRI often does not improve outcomes and may increase anxiety and unnecessary interventions.
The role of clinical examination
A proper neurological and orthopedic examination remains irreplaceable.
A neurosurgeon evaluates:
- muscle strength and reflexes;
- sensory changes;
- pain distribution patterns;
- posture and movement;
- correlation between symptoms and imaging.
MRI findings must confirm clinical suspicion, not replace it.
Why patients misinterpret MRI reports
MRI reports are written for clinicians, not patients. Terms such as “degenerative changes,” “protrusion,” or “compression” can be alarming when taken out of context.
Without professional explanation, patients may:
- overestimate the severity of findings;
- assume surgery is inevitable;
- restrict activity unnecessarily;
- develop fear-avoidance behaviors that worsen outcomes.
Education is a critical part of treatment.
MRI after surgery or treatment: another common pitfall
Post-treatment MRI findings often show residual changes that do not correlate with symptoms. Healing, scarring, and adaptation take time.
Repeating MRI without clinical indication may:
- confuse decision-making;
- prompt unnecessary interventions;
- distract from functional recovery.
Conclusion
MRI is a powerful diagnostic tool, but it does not diagnose pain by itself.
Back pain should never be treated based on imaging alone.
Effective management requires:
- clinical evaluation;
- understanding of pain mechanisms;
- careful interpretation of imaging;
- individualized treatment planning.
The most important question is not “What does the MRI show?” but “How do the findings relate to the patient?”


